Whether called fibrocystic breast “changes” or fibrocystic breast “disease”, it’s a problem that affects up to half of all women at some point during their lives. Currently, most doctors just refer to women as having fibrocystic breasts, since it really isn’t a disease at all. Fibrocystic breasts are lumpy, thick, and tender, especially right before menstruation. The condition primarily affects women between the ages of 30 and 50 and tends to become less of a problem after menopause.
 Why do breasts develop fibrocystic changes? Fibrocystic breast changes are linked to the hormone production that occurs during the menstrual cycle. There is no proof that drinking caffeine, eating chocolate, or eating a high fat diet is primarily responsible for this condition.
Why do breasts develop fibrocystic changes? Fibrocystic breast changes are linked to the hormone production that occurs during the menstrual cycle. There is no proof that drinking caffeine, eating chocolate, or eating a high fat diet is primarily responsible for this condition.
What symptoms are associated with fibrocystic breasts? Specific symptoms include breast soreness, swelling, and heaviness. Generalized breast lumpiness occurs most commonly in the upper/outer aspect of the breast (the portion closest to the armpit). Symptoms are generally worse right before the menstrual period, and then improve after menstruation begins. Women who take hormone replacement therapy often have more symptoms, whereas, women who take birth controls pills have fewer symptoms.
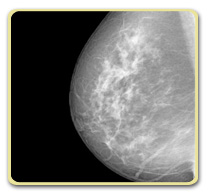
Is it necessary to undergo testing for fibrocystic breasts? In most cases, a history and physical examination that is consistent with fibrocystic breast changes, is adequate to make the diagnosis. If there are any worrisome lumps, such as those that persist through several cycles, a mammogram and/or ultrasound should be performed. Any new lump in a post-menopausal woman requires eval
uation, since this is unlikely to represent a fibrocystic change. In some cases, it may be necessary to obtain a sample (biopsy) of breast tissue with a needle or by surgery in order to make an accurate diagnosis and differentiate between a fibrocystic breast condition and breast cancer.
Is there a treatment for fibrocystic breasts? Treatment may not be necessary if symptoms are absent or tolerable. When painful, treatment is usually directed at the symptoms themselves, or at the hormonal changes that cause fibrocystic breasts. Symptomatic treatment includes taking a non-prescription analgesic, such as acetaminophen (e.g. Tylenol) or ibuprofen (e.g. Advil), use of heat or ice on the breast, and wearing a well-fitting bra. In some women, particularly those with irregular periods, taking low-dose birth control pills may be of benefit. In post-menopausal women on hormone replacement therapy, taking a periodic “vacation” from estrogen each month is sometimes beneficial.
Can fibrocystic breast changes develop into cancer? Fibrocystic changes pose no increased risk of developing cancer. However, fibrocystic breast changes can make it more difficult to distinguish developing breast cancer from fibrocystic lumps. Additionally, mammograms to screen for breast cancer can be more difficult to interpret when fibrocystic changes are present. This can lead to the increased need for additional testing such as ultrasound or biopsies.
Are natural remedies available for treating or preventing fibrocystic breasts? Certain “natural” treatments may work for some women, but none has been proven to help all women. These treatments include:
Caffeine avoidance, including chocolate, sodas, coffee, and tea.
Eating a low-fat diet, with fat constituting less than 15% of the day’s total calories.
Taking a vitamin E supplement
Using evening primrose oil, an oil that is high in gamma-linolenic acid.
Before taking any medication or supplement, particularly if you are on other medications or could be pregnant, it is best to talk with your doctor first.
Sources for article:
Fibrocystic Breasts from Mayo Clinic
Evening primrose oil for fibrocystic breasts from Cleveland Clinic Wellness
Fibrocystic Breast Disease from Medline Plus
Kent Davidson MD – Health Tip Content Editor
